Plantar Fasciitis: What You Need to Know for Recovery
Plantar fasciitis is a common condition that many people experience, especially those who are active. It typically causes stabbing pain in the bottom of the foot near the heel. This pain often worsens with the first steps in the morning or after long periods of sitting.
Understanding the causes and symptoms of plantar fasciitis can lead to effective treatment options. Many individuals may not realize that factors such as age, activity level, and foot mechanics can play a significant role in developing this condition.
Recognizing the symptoms early can help prevent the pain from becoming chronic. Effective management strategies exist that can provide relief and allow individuals to return to their daily activities with comfort.
Understanding Plantar Fasciitis
Plantar fasciitis is a common foot condition that leads to heel pain. It involves inflammation of the plantar fascia, a critical structure in the foot. Understanding its anatomy, causes, and risk factors can help in recognizing and treating this issue effectively.
Definition and Overview
Plantar fasciitis is characterized by pain in the heel or bottom of the foot. It results from irritation and inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot. This tissue connects the heel bone to the toes, supporting the arch and absorbing shock during walking.
Individuals often describe the pain as stabbing, especially with the first steps in the morning. The discomfort can lessen with movement but may return after long periods of standing or sitting. Many people seek treatment when the pain disrupts daily activities.
Anatomy of the Foot
The foot consists of three main parts: the forefoot, midfoot, and hindfoot. The plantar fascia primarily resides in the hindfoot and runs from the heel bone (calcaneus) to the toes. It plays a crucial role in maintaining the arch of the foot.
This tissue consists of dense connective tissue that can become inflamed due to overuse or strain. Other important structures include the muscles, ligaments, and bones that work together to support weight and provide balance during movement. Understanding this anatomy is vital for recognizing how plantar fasciitis develops.
Causes of Plantar Fasciitis
Several factors can cause plantar fasciitis. The most common cause is excessive strain on the plantar fascia. This strain may result from repetitive activities such as running or standing for long periods.
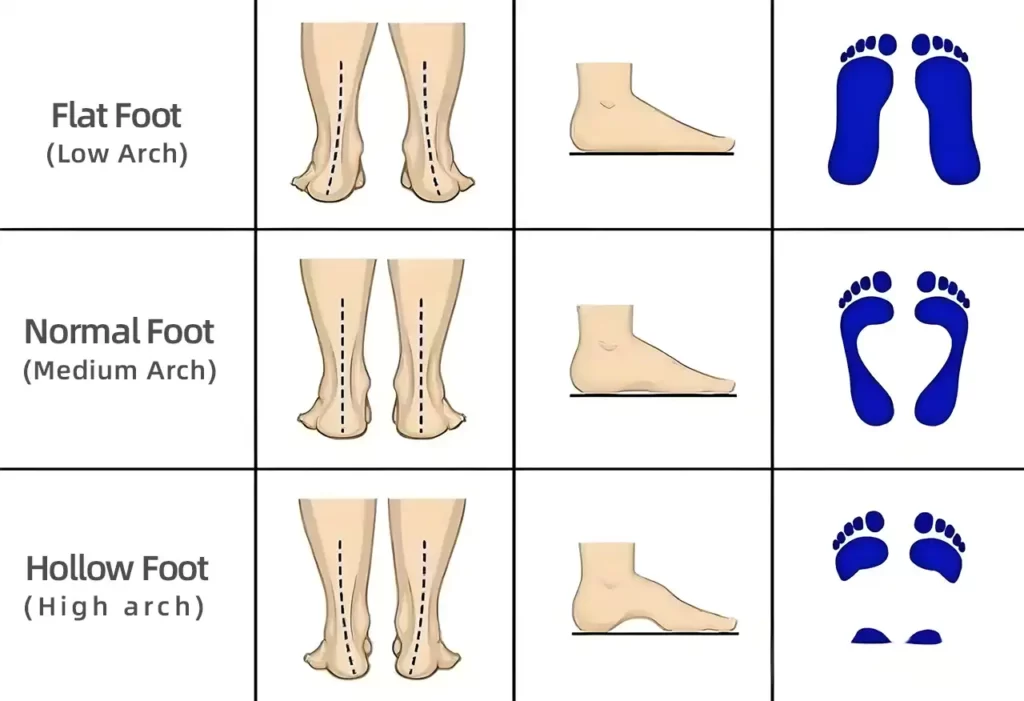
Other contributing factors include improper footwear that lacks support, high-impact sports, or flat feet. Patients may also experience increased pain after changes in activity, like starting a new exercise routine. Identifying these causes can help in effectively addressing and managing the condition.
Risk Factors
Certain risk factors increase the likelihood of developing plantar fasciitis. Age is a significant factor, as it often occurs in middle-aged adults. Individuals who are overweight may also experience more strain on their feet.
Occupations that require prolonged standing can lead to plantar fasciitis, as can sports that place excessive stress on the feet. Additionally, having tight calf muscles or a high arch can predispose a person to this condition. Awareness of these risk factors can aid in prevention and early intervention.
Symptoms and Diagnosis
Plantar fasciitis is a common foot condition characterized by specific symptoms. Accurate diagnosis is crucial for effective treatment. Understanding how to identify the symptoms and the diagnostic process can lead to better management of the condition.
Common Symptoms
The primary symptom of plantar fasciitis is pain at the bottom of the foot, especially near the heel. This pain is often most intense in the morning after waking up or after long periods of sitting. Patients may experience a sharp, stabbing feeling during the first steps of the day.
As the day progresses, the pain might decrease but can return after prolonged standing or physical activity. Swelling and tenderness along the arch of the foot may also occur. These symptoms can severely impact daily activities and overall quality of life.
Diagnostic Criteria
To diagnose plantar fasciitis, a healthcare professional will start with a thorough medical history and physical examination. They will check for:
- Tenderness in the heel and arch
- Range of motion in the foot and ankle
- Areas where pain is most acute
Diagnostic imaging, such as X-rays or MRIs, may be used to rule out other conditions. It is important for the doctor to assess patient symptoms and response to certain movements to confirm the diagnosis.
Differential Diagnosis
Differential diagnosis is important to rule out other conditions that may cause similar symptoms. Other conditions to consider include:
- Achilles tendonitis: Pain at the back of the heel instead of the bottom.
- Bursitis: Pain and swelling in the heel area.
- Heel spurs: Calcium deposits on the heel that can cause pain.
Differentiating between these conditions helps ensure appropriate treatment and management strategies. A correct diagnosis is vital for effective relief from pain and discomfort.
Treatment Options
There are several effective treatment options available for plantar fasciitis. These can help reduce pain and inflammation while improving mobility. Approaches range from conservative methods to more invasive surgical options.
Conservative Treatments
Conservative treatments focus on relieving pain and supporting the foot without aggressive interventions. These often include wearing orthotic devices that provide arch support. Patients are advised to avoid walking barefoot and using shoes with inadequate support.
Ice therapy is beneficial for reducing swelling. Patients can apply a cloth-covered ice pack to the affected area for 15 minutes several times daily. Stretching exercises for the calf muscles and plantar fascia can also improve flexibility and alleviate pain.
For footwear, it is essential to select shoes with good cushioning and arch support. Insoles or heel cups can provide extra comfort. Avoiding high-impact activities during recovery is recommended.
Physical Therapy
Physical therapy is a common treatment option for plantar fasciitis. It involves targeted exercises to strengthen the muscles in the foot and improve range of motion. A physical therapist can design a personalized exercise program.
Manual therapy techniques may also be employed. These include massage and joint mobilization to relieve tension in the plantar fascia. Stretching routines can enhance flexibility in the arches and calves.
Patients might learn proper walking techniques to avoid strain. Regular sessions can lead to significant pain relief and increased physical activity levels over time.
Medication and Pain Management
Medication plays a key role in managing pain associated with plantar fasciitis. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce inflammation. Patients may take these as needed for pain relief.

In some cases, doctors may prescribe stronger medications for persistent pain. Corticosteroid injections directly into the heel may provide temporary relief. These injections help reduce inflammation in the area.
It’s important to follow a healthcare provider’s guidelines on medication use. Misuse can lead to side effects or dependency. Engaging in a comprehensive treatment plan alongside medication is crucial for recovery.
Surgical Interventions
Surgery is considered when other treatment options fail to provide relief after a significant period, usually six months or longer. One common procedure is plantar fascia release, which involves cutting a portion of the fascia to relieve tension.
Another option is the removal of bone spurs if present. Surgery typically aims to alleviate pain while preserving foot function. Recovery from surgical interventions may take time, and patients often engage in physical therapy afterward.
Choosing surgery should be a well-informed decision made with a healthcare professional. Each case can vary widely, making personalized treatment plans essential.
Home Management
Managing plantar fasciitis at home involves specific exercises, suitable footwear, and lifestyle changes. These steps can help ease pain and improve overall foot health.
Exercises and Stretching
Exercises play a crucial role in relieving plantar fasciitis pain. Stretching the plantar fascia and calf muscles can reduce tension and improve flexibility.
One effective stretch is the calf stretch. To perform it, stand facing a wall, placing hands on the wall at eye level. Step back with one foot, keeping it straight. Bend the front knee. Hold for 15-30 seconds and switch feet.

Toe curls are another helpful exercise. Sit in a chair with a small towel on the floor. Use your toes to grab and pull the towel towards you. Repeat 10 times.
Regularly doing these exercises can promote healing and enhance mobility.
Footwear Advice
Choosing the right footwear is essential for managing plantar fasciitis. Supportive shoes can provide relief and prevent further injury.
Footwear should have good arch support and cushioning. Avoid flat sandals or high heels, as they can exacerbate pain. Look for shoes labeled as orthopedic or designed specifically for foot pain.
Inserts or orthotics can also boost support. They provide additional cushioning and help align the foot properly. This can alleviate stress on the plantar fascia.
It’s important to replace worn-out shoes regularly. This ensures that ample support is always maintained.
Lifestyle Modifications
Certain lifestyle changes can significantly impact plantar fasciitis management. Simple adjustments can help reduce strain on the feet.
Maintaining a healthy weight can lessen the pressure on the feet. If weight loss is necessary, a balanced diet and regular exercise can aid this goal.
Incorporating specific rest periods throughout the day can also be beneficial. Avoid prolonged standing or walking on hard surfaces. Whenever possible, take breaks to sit down and elevate the feet.
Using cold therapy can ease pain. Applying ice to the affected area for 15-20 minutes can reduce inflammation. It’s a simple and effective way to manage discomfort at home.
Prevention Strategies
Preventing plantar fasciitis involves a combination of specific exercises, maintaining a healthy weight, and ensuring proper foot mechanics. These strategies can help minimize the risk of developing this painful condition.
Preventive Exercises
Regular exercises can strengthen the muscles in the feet and provide better support for the plantar fascia. Stretching the foot and calf muscles is particularly important.
Some effective exercises include:
- Towel Stretch: Sit with your legs extended. Loop a towel around the ball of your foot and gently pull it towards you, stretching your calf and arch.
- Toe Curls: While sitting, place a towel on the floor and try to pull it towards you using your toes. This strengthens the arch muscles.
- Heel Raises: Stand holding onto a chair or wall for support. Raise your heels off the ground and lower them back down. This strengthens the calves and stabilizes the ankle.
Weight Management
Maintaining a healthy weight is crucial for foot health. Excess body weight puts additional stress on the plantar fascia, which can lead to inflammation and pain.

To manage weight effectively:
- Balanced Diet: Focus on a diet rich in fruits, vegetables, lean proteins, and whole grains. This helps support overall health and weight management.
- Regular Exercise: Engage in low-impact activities, such as swimming or cycling, to control weight without putting excessive stress on the feet.
- Hydration: Drink plenty of water, as staying hydrated helps maintain healthy body function and may support weight control.
Proper Foot Mechanics
Ensuring proper foot mechanics can greatly reduce the risk of plantar fasciitis. Wearing appropriate footwear is vital.
Key factors include:
- Supportive Shoes: Choose shoes that offer good arch support and cushioning. Avoid walking barefoot on hard surfaces.
- Orthotic Inserts: Consider wearing orthotic inserts if foot structure issues like overpronation occur. These can provide additional support to the arch and heel.
- Footwear Fit: Ensure shoes fit well. They should not be too tight or too loose, as ill-fitting shoes can cause unnecessary strain on the plantar fascia.
Complications and Prognosis
Plantar fasciitis can lead to various complications if left untreated. Understanding these risks is important for managing symptoms effectively. The long-term outlook for individuals with this condition varies based on treatment and adherence.
Potential Complications
If plantar fasciitis is not addressed, individuals may face several complications. Chronic pain in the heel can develop, making daily activities challenging. Over time, lack of mobility can result in decreased physical fitness, leading to weight gain or other health issues.
Other serious complications may include plantar tears, where the fascia experiences significant damage. This can cause sharp, intense pain and may require surgical intervention. Patients might also experience changes in walking patterns due to the pain, which can lead to additional issues in the knees, hips, or lower back.
Long-Term Outlook
The prognosis for plantar fasciitis depends on various factors, including treatment effectiveness and individual commitment to rehabilitation. Most people respond well to conservative treatments like physical therapy, stretching, and orthotics.
With proper care, many patients experience relief within six to twelve months. However, neglecting treatment can lead to prolonged discomfort and a higher risk of complications.
In rare cases, some individuals may need surgery if other treatments fail. Early diagnosis and proper management are critical for a favorable long-term outlook.
Current Research
Current research on plantar fasciitis focuses on new treatments and recent findings that shed light on this common condition. The aim is to improve patient outcomes and understand the underlying causes better.
Emerging Treatments
Recent studies have explored various innovative treatments for plantar fasciitis. Extracorporeal Shock Wave Therapy (ESWT) has gained attention. This non-invasive method uses sound waves to reduce pain and promote healing. Research has shown that ESWT can significantly decrease discomfort and improve functionality in patients.
Another area of interest is the use of platelet-rich plasma (PRP) injections. This approach involves injecting a concentration of platelets from the patient’s blood into the affected area. Early results indicate that PRP can enhance healing and reduce inflammation in the plantar fascia, offering hope for chronic cases.
Recent Findings
Recent findings have highlighted the prevalence and impact of plantar fasciitis. It accounts for around 1 million doctor visits each year in the United States. Most patients presenting with heel pain receive a diagnosis of this condition.
A systematic review revealed trends in the epidemiology of plantar fasciitis. It is more common in individuals who are overweight or engaged in high-impact sports. A study noted that nearly two-thirds of people with plantar foot pain consulted a healthcare professional within the past year. This underscores the growing awareness and need for effective management strategies.
Frequently Asked Questions
Understanding plantar fasciitis can help in finding relief from heel pain. The following information addresses common concerns and offers insights into treatment options, exercises, and footwear.
What are the most effective treatments for heel pain associated with this condition?
The most effective treatments for heel pain include rest, ice application, and over-the-counter pain relievers. Physical therapy may also provide targeted exercises to strengthen the foot. In some cases, custom orthotics can help support the arch and reduce pain.
What exercises can help with relieving discomfort in the foot’s arch and heel?
Stretching exercises are beneficial for relieving discomfort. Heel stretches, calf stretches, and foot rolls using a golf ball or frozen bottle can help. These exercises improve flexibility in the plantar fascia and reduce tension.
How can one manage symptoms of this condition at home?
Home management of plantar fasciitis symptoms includes using ice packs on the affected area, resting the foot, and performing gentle stretches. Elevating the foot and avoiding walking on hard surfaces can also aid in reducing pain.
What footwear is recommended to alleviate the stress on the heel and arch?
Footwear that provides arch support and cushioning is recommended. Shoes with a firm heel counter and a cushioned insole can help absorb shock. Avoiding flat shoes or high heels is important for preventing added stress on the plantar fascia.
What symptoms indicate the presence of this inflammatory condition of the foot?
Symptoms of plantar fasciitis include sharp heel pain, especially with the first steps in the morning or after sitting. Pain may also intensify after standing for long periods. Swelling and tenderness along the arch of the foot can also indicate this condition.
How long does it typically take for the pain in the heel and arch to subside?
The duration for heel pain to subside varies. With consistent treatment, symptoms often improve within a few weeks to a couple of months. Severe cases may take longer, especially if the condition is not effectively managed.







